Quick Safety 51: Proactive prevention of maternal death from maternal hemorrhage
Issue:
In the United States, approximately 700 women die annually from pregnancy-related complications — a shocking statistic considering that most pregnancy-related deaths are preventable.1 The most frequent cause of severe maternal morbidity and preventable maternal mortality is obstetric hemorrhage — excessive blood loss from giving birth.2 Recent data indicate that rates of maternal hemorrhage are increasing in developed countries, including the U.S. Also, the rate of hemorrhage-associated severe maternal morbidity (defined as the need for blood transfusion of four or more units of packed red blood cells and/or ICU level care during the birth process or immediate postpartum period) has exceeded the morbidities associated with other obstetric or medical conditions that may result in complications requiring higher level of care.
In addition, there are significant racial/ethnic disparities in pregnancy-related mortality; black women have a pregnancy-related mortality ratio approximately three times as high as that of white women.3,4 Fully addressing these unacceptable mortality rates will require truly understanding the contributing factors that lead to mortality in African American women and other disproportionately affected populations in order to develop focused solutions. Overall, better understanding is needed on the circumstances surrounding pregnancy-related deaths and strategies to prevent future deaths.
As a result of this significant patient safety concern, The Joint Commission introduced two new standards, effective July 1, 2020, to address complications in maternal hemorrhage and severe hypertension/ preeclampsia. This Quick Safety provides background information around strategies for the management of maternal hemorrhage that are outlined in new Provision of Care, Treatment, and Services standard PC.06.01.01: Reduce the likelihood of harm related to maternal hemorrhage.
Maternal mortality by the numbers
Maternal hemorrhage is defined by the American College of Obstetricians and Gynecologists (ACOG) as a cumulative blood loss of greater than or equal to 1,000 mL, or blood loss accompanied by signs or symptoms of hypovolemia, within 24 hours after the birth process.5 Approximately 3-5% of obstetric patients will experience a postpartum hemorrhage.6 These preventable events are the cause of 27% of maternal deaths worldwide,7 and 11.2% of U.S. maternal deaths.8
A review of the Joint Commission sentinel event database for cases coded as maternal death or severe maternal morbidity for 2010 through August 2019, indicate maternal hemorrhage is a causal factor in 51% of those reported sentinel events.
During 2011-2015, the Centers for Disease Control and Prevention (CDC) reports 3,410 pregnancy-related deaths occurred in the U.S., and the overall pregnancy-related mortality ratio was 17.2% pregnancy-related deaths per 100,000 live births.8 When combined, cardiovascular conditions were responsible for more than 33% of pregnancy-related deaths; these conditions include cardiomyopathy (10.8%), other cardiovascular conditions (15.1%), and cerebrovascular accidents (7.6%). Other leading causes of pregnancy-related death included other noncardiovascular medical conditions (14.3%), infection (12.5%), and obstetric hemorrhage (11.2%).8
 According to the CDC, the rate of postpartum hemorrhage with procedures to control hemorrhage per 10,000 delivery hospitalizations increased from 4.3 in 1993 to 21.2 in 2014, with sharper increases in later years. The rate of postpartum hemorrhage with blood transfusions also increased noticeably over time, from 7.9 in 1993 to 39.7 in 2014.9
According to the CDC, the rate of postpartum hemorrhage with procedures to control hemorrhage per 10,000 delivery hospitalizations increased from 4.3 in 1993 to 21.2 in 2014, with sharper increases in later years. The rate of postpartum hemorrhage with blood transfusions also increased noticeably over time, from 7.9 in 1993 to 39.7 in 2014.9
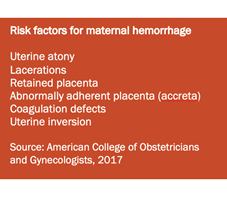
Although common risk factors for postpartum hemorrhage are known (see sidebar), it is important to note that 20% of hemorrhages occur in women with no risk factors. All members of the obstetrical care team must maintain a constant readiness for this often-unpredictable emergency. Maintaining situational awareness and preoccupation with failure are cornerstones of high-reliability thinking and are critical components of care strategies in today’s fast-paced clinical care areas.
Using obstetric hemorrhage bundles
Strategies to reduce morbidity and mortality from postpartum hemorrhage have included the use of standardized, comprehensive, obstetric safety bundles.2 A patient safety bundle is a set of evidence-based recommendations for practice and care processes known to improve outcomes.2 Standardization and reduced variation have been shown to improve outcomes and quality of care.
To help promote standardization of health care processes, the Council on Patient Safety in Women’s Health Care — representing all major women’s health care professional organizations — has developed for dissemination an obstetric hemorrhage safety bundle. Implementing these evidence-based safety bundles has been shown to demonstrate significant reductions in maternal morbidity.2 The consensus bundle on obstetric hemorrhage is organized into four action domains: Readiness, Recognition and Prevention, Response, Reporting and Systems Learning.
Safety actions to consider:
Applying high reliability principles — such as preoccupation with failure, reluctance to simplify operations, and ongoing situational awareness — can be operationalized with the consistent use of safety bundles. The safety actions below are based on the Council on Patient Safety in Women’s Health Care obstetric hemorrhage patient safety bundle.10 This bundle is not a new guideline, but rather represents existing guidelines and recommendations in a form that aids consistent practice.2 The goal of implementing the safety bundle is to improve outcomes for women and infants.
Recognizing all members of the health care team have vital roles in guiding women through their birth experience represents a challenge to some organizations. Working as a team, with the end goal of safety for all who are touched by the birth experience, will help to improve the health and well-being of organizations, communities and the world.
Readiness — Every Obstetric Unit
- Have a standardized, secured, and dedicated hemorrhage supply kit10 that must be stocked per the hospital’s defined process and, at a minimum, contains:
- Emergency hemorrhage supplies as determined by the hospital.
- The hospital’s approved procedures for severe hemorrhage response.
- Provide immediate access to hemorrhage medications.10
- Establish response team — who to call when help is needed.10
- Provide role-specific staff education on your organization’s hemorrhage policies at regular intervals, including new employee orientation, whenever policy is changed, or every two years.
- Establish massive transfusion emergency release protocol.10
- Conduct multidisciplinary annual drills and debrief on hemorrhage response procedures.10
Recognition — Every Patient
- Assess hemorrhage risk — prenatal, on admission, or other appropriate times.10
- Provide education to patient and family on signs and symptoms of postpartum hemorrhage while in the hospital and at home after discharge.
Response — Every Hemorrhage
- Establish a standardized, obstetric hemorrhage emergency management plan.10
- Provide guidance on how to communicate with patients and families during and after the event.
Reporting/Systems Learning — Every Unit
- Establish a culture of huddles for high-risk patients and post-event debriefs to identify success and opportunities for improvement.10
- Conduct a multidisciplinary review of hemorrhages that meet established criteria for evaluation of effectiveness of treatment and services provided by the hemorrhage response team.10
- Monitor outcomes and process metrics via your organization-determined quality improvement committee.10
Resources:
1. Building U.S. Capacity to Review and Prevent Maternal Deaths. Report from nine maternal mortality review committees. 2018.
2. Main E, et al. National Partnership for Maternal Safety Consensus Bundle on Obstetric Hemorrhage. Obstetrics & Gynecology, 2015;126(1)155-162.
3. Creanga AA, et al. Pregnancy-Related Mortality in the United States, 2011-2013. Obstetrics & Gynecology, 2017;130:366-73.
4. CDC. Pregnancy Mortality Surveillance System. Atlanta, GA: U.S. Department of Health and Human Services, CDC, 2019.
5. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin Number 183, Postpartum Hemorrhage. Obstetrics & Gynecology, 2017;130(4)e168-1186.
6. Evensen A, et al. Postpartum Hemorrhage: Prevention and Treatment. American Family Physician, 2017;95(7)442-448.
7. International Federation of Gynecology and Obstetrics (FIGO). PPH Leading to Unnecessary Deaths. June 14, 2018.
8. CDC. Morbidity and Mortality Weekly report, 2019;68(18)423-29.
9. CDC. Data on Selected Pregnancy Complications in the United States. Atlanta, GA: U.S. Department of Health and Human Services, CDC, 2019.
10. Council on Patient Safety in Women’s Health Care. Patient Safety Bundle Obstetric Hemorrhage, May 2015.
Note: This is not an all-inclusive list.


