Quick Safety 43: Managing medical device-related pressure injuries
Issue:
Pressure injuries (which were called pressure ulcers) are not new to health care, but more of these injuries are being caused by medical devices. Medical device-related pressure injuries now account for more than 30 percent of all hospital-acquired pressure injuries.1 Compounding the problem is the difficulty staff have in differentiating medical device-related injuries from those caused by immobility. Both types of pressure injuries are frequently found over bony prominences. While immobility-related pressure injuries occur to tissue exposed to pressure from a support surface, medical device-related pressure injuries often mirror the shape and location of a device.2 See examples in the “Best Practices for Prevention of Medical Device-Related Pressure Injuries,” from the National Pressure Injury Advisory Panel (NPIAP).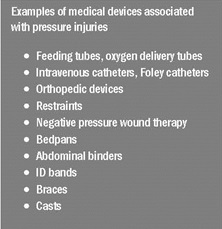
Almost every hospital patient requires at least one medical device for their care and treatment. Consequently, every patient with a medical device is at risk for pressure injuries due to impaired sensation, poor perfusion, altered tissue tolerance, poor nutrition, edema, and the tendency for moisture to develop under devices. Prevention and management of medical device-related pressure injuries are difficult, because the device cannot always be moved or removed.
These devices are often rigid, and size and selection of the medical device can affect the pressure on the skin.3 Examples of devices associated with pressure injuries include feeding tubes, oxygen delivery devices, intravenous catheters, orthopedic devices, and many others that assist patients with their daily routine and needs.
Quick Safety Issue 25: “Preventing pressure injuries,” provides prevention strategies for and definitions of all types of pressure injuries, based on guidance from the NPIAP's Consensus Conference in April 2016.4 This Quick Safety builds on the information in Issue 25, providing specific guidance to help health care professionals manage pressure injuries from the use of medical devices.
Historically, preventing and treating health care-acquired pressure injuries have been a challenge for health care organizations due to the:
- Pain they cause.
- Increased risk of infection.
- Need for additional care and treatment related to the pressure injury.
- Patient’s altered body image.
- Impact to the patient’s disease process.
Treatment of pressure injuries can be costly, and is devastating to caregivers as well as to the patient. Most pressure injuries occur over bony prominences, such as the heels and the sacrum. However, the NPIAP recognizes pressure injuries also can occur on any tissue under pressure and thereby can develop beneath medical devices.5
While there’s little published data on medical device-related pressure injuries, they are known to be a significant cause of patient morbidity. Many pressure injuries are preventable with the use of evidence-based nursing practice, but identifying and preventing medical device-related pressure injuries is difficult, since the need for the device can be crucial, especially for patients with deteriorating condition(s).
Safety actions to consider:
Early identification and intervention is key to managing medical device-related pressure injuries. The following suggested actions can be taken by health care professionals to help their patients who suffer from these debilitating injuries.
1. Assessment: A comprehensive skin assessment can lead to proper identification and early prevention. It is critical to assess the skin underneath a medical device to identify the early signs of pressure. Pressure injury risk assessment is a standardized process that is aided by the use of risk assessment tools or scales. To identify patients at risk for pressure injuries, validated risk assessment tools typically evaluate several different dimensions of risk (such as mobility, nutrition and moisture) and assign points depending on the extent of any impairment.6
2. Education: Consider educating the patient and family about what the device is, where it is located, why it is there, how it functions, and how long it will stay in place. Awareness is key.
3. Positioning: Position and reposition the patient and the device to help redistribute pressure and decrease shear force. Determine repositioning frequency with consideration of the patient’s general medical condition, comfort, and level of activity and mobility. Remove the device as soon as medically feasible.
4. Device care: Ensure that the patient receives the proper size and type of device; that the device is secure, to decrease movement or slippage; that the skin is padded, to reduce friction; and that the manufacturer’s recommendations for use and care of the device are followed.
5. Documentation and communication: Ensure that the patient’s assessment, interventions and continuing care needs are passed from one caregiver to the next. Use of standardized forms, tools, methods and technologies can help caregivers communicate more effectively and make successful hand-offs.
6. Teamwork: Pressure injury prevention requires activities and coordination among many individuals, including the multiple disciplines and many teams involved in developing and implementing the patient’s care plan. High-quality prevention requires an organizational culture and operational practices that promote teamwork and communication, as well as recognize individual expertise. Therefore, improvement in pressure injury prevention calls for a system focus to make needed changes.7
7. Continuous monitoring: Observe baseline and progression or healing over time. Pressure injuries are painful, and patients are suffering more than health care providers know. Consider performing periodic physical, psychological and psychosocial reassessments of the patient. Ask questions and look for non-verbal cues of pain and discomfort. Monitor incidence and prevalence of medical device-related pressure injuries in your organization. Benchmark with other organizations, and share the results with staff.
Resources:
1. Health Research & Educational Trust. Hospital Acquired Pressure Ulcers/Injuries (HAPU/I): April 2017. Chicago, IL: Health Research & Educational Trust.
2. Black J and Kalowes P. Medical device-related pressure ulcers. Chronic Wound Care Management and Research. 2015;(3):91-99.
3. National Pressure Injury Advisory Panel website. Educational and Clinical Resources. Best practices for prevention of medical device-related pressure injuries posters. Washington, DC: National Pressure Injury Advisory Panel.
4. The Joint Commission. Preventing pressure injuries. Quick Safety. Issue 25, July 2016. Oakbrook Terrace, IL: The Joint Commission.
5. National Pressure Injury Advisory Panel website. NPIAP Pressure injury stages. Washington, DC: National Pressure Injury Advisory Panel.
6. Agency for Healthcare Research and Quality. Preventing pressure ulcers in hospitals: A toolkit for improving quality of care. Rockville, MD: Agency for Healthcare Research and Quality.
7. Agency for Healthcare Research and Quality. Preventing Pressure Ulcers in Hospitals. Rockville, MD: Agency for Healthcare Research and Quality.
Note: This is not an all-inclusive list.


