Update: May 2022
Issue:
Unintended retained foreign objects (URFOs) were the most frequent sentinel event reported to The Joint Commission’s Sentinel Event database for 2017 and 2018 and the second most frequent event reported in 2019 and 2020. For 2021, 97 cases were reported, making it the third most common sentinel event reported to The Joint Commission. This downward trend shows that further vigilance is needed to mitigate risks and prevent this harm event from reaching a patient.
In October 2013, The Joint Commission issued a Sentinel Event Alert that addressed the prevention of URFOs.1 That alert listed the most common root causes of URFOs reported to The Joint Commission, which continue to be:
- The absence of policies and procedures
- Failure to comply with existing policies and procedures
- Problems with hierarchy and intimidation
- Failure in communication with physicians
- Failure of staff to communicate relevant patient information
- Inadequate or incomplete education of staff
A more recent review of data through 2020 indicates the most frequent root causes to be leadership, human factors and communication.
Safety Actions to Consider:
Hospitals, office-based surgeries and other facilities that conduct invasive procedures can help detect and prevent URFOs by creating, implementing, and communicating policies and procedures specific to URFOs, and ensuring their effectiveness by tracking compliance. Organizations can help ensure success by involving the entire procedure team in developing performance expectations regarding the detection and prevention of URFOs, which should be addressed in the policies and procedures. In addition, each member of the medical staff must be aware of his or her role in eliminating URFOs. Physicians should be part of any safety culture initiative, including high reliability training, project involvement and engagement surveys.
This issue of Quick Safety builds on Sentinel Event Alert issue 51. The following strategies to prevent URFOs were published in the June2 and July3 2015 issues of Joint Commission Resources’ The Source.
To prevent URFOs, organizations should address the following:
Count process
- Standardize count policies for all procedures – not just those involving an open chest or abdomen. Having different count expectations depending on the type of procedure can lead to URFOs.
- Policy should describe expected behavior and staff engagement while performing the count process, including required actions for an incorrect count that cannot be reconciled.
- Establish uniform documentation of the count process across all procedural areas, including areas where emergent procedures – such as central line insertion – may be performed (e.g., ED, ICU or at the bedside on a nursing unit). Communicate and educate staff on the established process for documentation, including its application to all procedures. Collect data to verify consistent use of the new processes in applicable areas and to monitor compliance.
- Make it the entire team’s responsibility to reconcile the count. If a team member believes the count should be repeated, the team should support this request.
- Consider how to handle counts for breaks or shift changes. For example, some organizations require full counts when staff change for a lunch break.
- Assess competency of the count process prior to the completion of orientation. Reassess this competency annually in order to identify process deviations and policy drift.
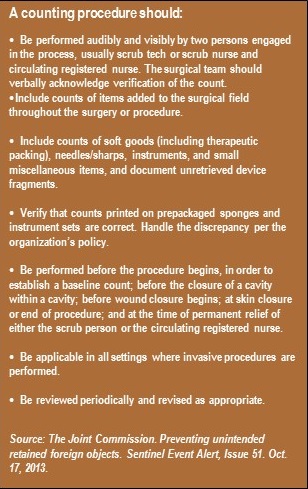
Note: See the sidebar for more information on the count procedure.
Team communication and interaction in the OR
- Policies that include physician-staff interaction should clearly state important behavioral and verbal expectations, which may include:
- Physician voices affirmation that count is correct prior to completion of skin closure.
- Calling out when an instrument is placed into a body cavity and not immediately removed; this enables the circulator to note and track that instrument through the completion of the case.
- Verbal affirmation by the team that the patient meets criteria for an intraoperative X-ray to screen for URFOs.
- When policy deviation occurs, staff should be educated about and comfortable speaking up, stopping the line, and escalating issues up the chain of command. Policies should provide clear direction on the escalation process.
Tools and methods used during a procedure
- Tools to help manage equipment and materials include white boards, sponge trees, radio-frequency identification (RFID) technology, radio-opaque supplies, and count documentation methodology. Each organization will need to select the best method(s) based on its priorities, such as ease-of-use or cost.
- Selected tools should be consistently available in the areas where invasive procedures are performed.
- Monitor compliance with tool usage and hold staff accountable for using tools consistently.
Physical environment
- Standardize the layout of procedural areas. The location of a particular procedure may not be consistent, due to scheduling issues or emergent cases. Teams that are working in a new or unfamiliar location will engage better if the environment has comparable equipment located in similar locations.
- Adjust lighting levels to enhance visibility. Low lighting can prevent adequate inspection of instruments and affect the visibility of white board information.
- Limit the number of people in the procedure room. Before the onset of the procedure, assess observers and other non-essential staff to determine if they need to be in the room. The number of people in the procedure room can affect noise levels and visibility and distract staff.
Radiology
- Identify any conditions that require an X-ray. For example, emergent cases in which counts were not performed.
- Any object or structure on a film that cannot be clinically correlated with current patient information should be treated as a critical result. It should generate a call between the radiologist and the physician of record.
- Policy language should be clear on the communication that should take place between the OR and radiology when an intraoperative X-ray is performed – most notably, why the X-ray is being performed (i.e., potential URFO). Both the surgeon and the radiologist should review the completed film.
Reporting of the discovery of a URFO
- Reporting of a discovered URFO should take place regardless of where the URFO occurred. For example, URFOs discovered in the private physician’s office as a result of a procedure performed in the hospital should be reported to that hospital.
- Reporting systems should be nonpunitive, with a clearly stated goal that reporting provides the opportunity for analysis so the system or process failure can be identified, investigated and mitigated.
Resources:
1. The Joint Commission. Preventing unintended retained foreign object Sentinel Event Alert, Issue 51. Oct. 17, 2013.
2. Anderson-Drevs, KS. Lessons learned: Preventing patient safety events involving unintended retained foreign objects, Part 1. Joint Commission Resources. The Source 13(6); June 2015 (accessed Oct. 5, 2015).
3. Anderson-Drevs, KS. Lessons learned: Preventing patient safety events involving unintended retained foreign objects, Part 2. Joint Commission Resources. The Source 13(7); July 2015.
Other resources:
- Steelman VM, Shaw C, Shine L Hardy-Fairbanks AJ. Unintentionally Retained Foreign Objects: A Descriptive Study of 308 Sentinel Events and Contributing Factors. Joint Commission Journal on Quality and Patient Safety 2019; 45:249-258.
- Wallace SC. Retained Surgical Items: Events and Guidelines Revisited. Pennsylvania’s Patient Safety Authority. 2017 March;14(1)27-35.
Note: This is not an all-inclusive list.