Built Environment - Clinical Impact
This content includes information linking Environment of Care and Life Safety Code deficiencies and their impact on patient care and patient safety.
EC.02.06.01: The organization establishes and maintains a safe, functional environment
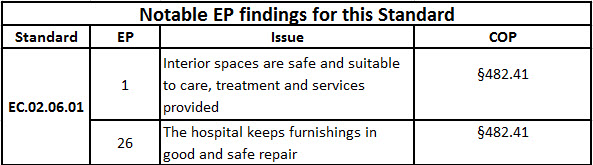
Clinical Impact - EP 1:
Interior spaces meet the needs of the patient population and are safe and suitable to the care, treatment and services provided.
Safe interior spaces. Patients and staff assume when they come to our facilities that the physical environment will be safe. But what about that small tear in the carpet? This potential trip hazard is unsafe, and could cause any patient, visitor or staff to become injured. Who is responsible for managing this? We have already discussed corridor clutter in Module 2, where general clutter (including equipment left unattended in the corridor, such as IV poles, med carts, linen collection hampers, etc.) creates an unsafe environment for patients, visitors or staff. One proposed solution is improving the Safety Culture, using a “Safety First” approach.
Any unsafe condition will be cited at EC.02.06.01 EP 1.This EP is equivalent to the OSHA General Duty Clause, which states that “each employer shall furnish to each of his employees employment and a place of employment which are free from recognized hazards...” This clause is used by OSHA whenever any unsafe condition is identified that does not have a correlating rule or regulation. The Joint Commission uses this EP similarly.
Maintaining a safe physical environment is everyone’s responsibility, which is more than just a cliché. In our healthcare environment each of us must be sensitive to potential risks to one another, including where the risk came from. In one nursing unit a staff member was walking down the corridor and saw a puddle of water. They immediately went and got a towel to wipe it up. Later that afternoon a someone else was walking in the unit, slipped on water and injured their hip. Did the person who first wiped up the water fail to exhibit a safety awareness? No, of course not. But what can we learn from this? The first person, acting correctly in removing the risk [water] failed to find the source and take appropriate corrective action.
To make reporting of unsafe conditions easier for staff, the use of Safety Champions can be extremely helpful. Also, as staff rotate through the Safety Champion program a heightened sense of safety will develop. The Safety Champion program has one person from each unit/department specifically trained in safety awareness according to organization policy and unit/department policy. General safety education is also stressed to those participating. One of the responsibilities of the Safety Champion is conducting the Environment of Care Tours, which is one way for staff to identify and seek corrective actions for possible unsafe conditions. For more on Safety Champions see Perspectives, February 2013.
Another concern related to the physical environment is hospital-acquired infections (HAI). Coming in at fourth place in the CDC list of causes of HAI is the physical environment. CDC has stated, “There were an estimated 722,000 HAIs [Healthcare-Associated Infections] in U.S acute care hospitals in 2011. About 75,000 hospital patients with HAIs died during their hospitalizations. More than half of all HAIs occurred outside of the intensive care unit.” [CDC Data & Statistics Web Page, 5/13/2015]
Unsafe practice can contribute to these numbers. Certainly ensuring the equipment and clinical areas are clean and suitable for patient care is important. Clinical Alarm management is also important.


